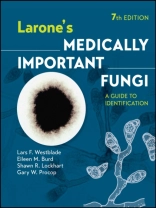
Larone’s
MEDICALLY IMPORTANT FUNGI
The definitive guide for identifying fungi from clinical specimens
With a new team of authors, Larone’s Medically Important Fungi, Seventh Edition, continues the longstanding tradition of high-quality content to expand your knowledge and support your work in clinical mycology by:
- Providing detailed descriptions of the major mycoses as viewed in patients’ specimens by direct microscopic examination of stained slides
- Offering a logical step-by-step process for identification of cultured organisms, utilizing detailed descriptions, images, pointers on organisms’ similarities and distinctions, and selected references for further information
- Covering more than 150 of the fungi most commonly encountered in the clinical mycology laboratory, including new entries for Emergomyces, Metarhizium anisopliae, Rasamsonia argillacea, Rhinocladiella mackenziei, Schizophyllum commune, and Thermothelomyces thermophilus
- Presenting details on each organism’s pathogenicity, growth characteristics, relevant biochemical reactions, and microscopic morphology, illustrated with photomicrographs, unique and elegant drawings, and color photos of colony morphology and various test results
- Explaining changes in fungal taxonomy and nomenclature that are due to information acquired through molecular taxonomic studies of evolutionary fungal relationships
- Providing basic information on molecular diagnostic methods, e.g., nucleic acid amplification and sequencing, MALDI-TOF mass spectrometry, and other commercial platforms
- Including an extensive section of easy-to-follow lab protocols, a comprehensive list of media and stain procedures, guidance on collection and preparation of patient specimens, and an illustrated glossary
With Larone’s Medically Important Fungi: A Guide to Identification, both novices and experienced professionals in clinical microbiology laboratories can confidently identify commonly encountered fungi.
Spis treści
List of Tables xvii
Preface to the Seventh Edition xix
Preface to the First Edition xxi
Acknowledgments xxiii
About the Authors xxv
Basics 1
How To Use the Guide 3
Use of Reference Laboratories and Regulations for Transport 5
Safety Precautions 11
Taxonomy and Nomenclature 13
Part I Direct Microscopic Examination of Clinical Specimens 15
Introduction 17
Histological Terminology 21
Tissue Reactions to Fungal Infection 25
Stains 29
Table 1.1 Histochemical stains for fungi and/or filamentous bacteria in tissue 30
Guide to Interpretation of Direct Microscopic Examination 33
Detailed Descriptions 39
Actinomycosis 40
Mycetoma (Actinomycotic or Eumycotic) 41
Nocardiosis 43
Mucormycosis (Zygomycosis) 44
Aspergillosis 45
Miscellaneous Hyalohyphomycoses (Other than Aspergillosis) 47
Dermatophytosis (Tinea, Ringworm) 49
Tinea versicolor 50
Tinea nigra 51
Phaeohyphomycosis 52
Chromoblastomycosis 53
Sporotrichosis 54
Histoplasmosis 55
Emergomycosis 57
Talaromycosis (Penicilliosis) 58
Blastomycosis 59
Paracoccidioidomycosis 60
Lobomycosis 61
Candidiasis 62
Trichosporonosis 64
Cryptococcosis 65
Pneumocystosis 67
Protothecosis 68
Coccidioidomycosis 69
Rhinosporidiosis 70
Adiaspiromycosis 72
Part II Identification of Fungi in Culture 73
Guide to Identification of Fungi in Culture 75
Detailed Descriptions 105
Filamentous Bacteria 107
Introduction to Filamentous Bacteria 109
Table 2.1 Differentiation of filamentous aerobic actinomycetes encountered in clinical specimens 110
Nocardia spp. 111
Streptomyces spp. 114
Actinomadura spp. 116
Nocardiopsis dassonvillei 117
Yeasts and Yeastlike Organisms 119
Introduction to Yeasts and Yeastlike Organisms 121
Candida albicans 123
Table 2.2 Characteristics of the genera of clinically encountered yeasts and yeastlike organisms 124
Candida dubliniensis 125
Table 2.3 Characteristics of Candida spp. most commonly encountered in the clinical laboratory 126
Table 2.4 Characteristics that assist in differentiating Candida dubliniensis from Candida albicans 128
Candida tropicalis 129
Candida parapsilosis species complex 130
Candida lusitaniae 131
Candida krusei 132
Table 2.5 Differentiating characteristics of Magnusiomyces capitatus (formerly Blastoschizomyces capitatus) versus Candida krusei 134
Table 2.6 Differentiating characteristics of Candida krusei, Candida inconspicua, and Candida norvegensis 134
Candida kefyr 135
Candida rugosa species complex 136
Candida guilliermondii species complex 138
Table 2.7 Differentiating characteristics of Candida guilliermondii versus Candida famata 139
Candida lipolytica 140
Candida zeylanoides 141
Candida glabrata species complex 142
Candida auris 143
Candida haemulonii species complex 144
Candida pelliculosa 145
Cryptococcus neoformans species complex 147
Cryptococcus gattii species complex 149
Table 2.8 Characteristics of Cryptococcus spp. and former members of the genus 150
Table 2.9 Characteristics of yeasts and yeastlike organisms other than Candida spp. and Cryptococcus spp. 151
Rhodotorula and Cystobasidium spp. 152
Sporobolomyces salmonicolor 154
Saccharomyces cerevisiae 156
Malassezia spp. 158
Malassezia pachydermatis 160
Ustilago spp. 161
Prototheca spp. 162
Trichosporon and Cutaneotrichosporon spp. 163
Table 2.10 Key characteristics of the most common clinically encountered Trichosporon spp. and Cutaneotrichosporon spp. 165
Magnusiomyces capitatus (formerly Blastoschizomyces capitatus) 166
Geotrichum candidum 167
Thermally Dimorphic and/or Endemic Fungi 169
Introduction to Thermally Dimorphic and/or Endemic Fungi 171
Histoplasma capsulatum 172
Emergomyces spp. 175
Blastomyces dermatitidis/gilchristii 177
Coccidioides immitis/posadasii 179
Paracoccidioides brasiliensis 181
Talaromyces marneffei (formerly Penicillium marneffei) 183
Sporothrix schenckii species complex 186
Emmonsia crescens 189
Thermally Monomorphic Moulds 191
Mucormycetes 193
Introduction to Mucormycetes 195
Table 2.11 Differential characteristics of similar organisms in the class Mucormycetes 197
Table 2.12 Differential characteristics of the clinically encountered Rhizopus spp. 197
Rhizopus spp. 198
Mucor spp. 200
Rhizomucor spp. 201
Lichtheimia corymbifera species complex 202
Apophysomyces elegans species complex 204
Saksenaea vasiformis 206
Cokeromyces recurvatus 207
Cunninghamella bertholletiae 209
Syncephalastrum racemosum 211
Basidiobolus spp. 212
Conidiobolus coronatus 213
Dematiaceous Fungi 215
Introduction to Dematiaceous Fungi 217
Fonsecaea spp. 218
Myrmecridium schulzeri 221
Rhinocladiella mackenziei (formerly Ramichloridium mackenziei) 222
Phialophora verrucosa 223
Table 2.13 Characteristics of Phialophora, Pleurostoma (formerly Pleurostomophora), Phaeoacremonium, Acremonium and Sarocladium, Phialemonium, and Coniochaeta (formerly Lecythophora) 224
Pleurostoma richardsiae (formerly Pleurostomophora richardsiae) 225
Phaeoacremonium parasiticum 226
Phialemonium spp. 228
Cladosporium spp. 230
Table 2.14 Characteristics of Cladosporium spp. and Cladophialophora spp. 232
Cladophialophora carrionii 233
Cladophialophora boppii 235
Cladophialophora bantiana 236
Scedosporium apiospermum species complex 237
Table 2.15 Differentiating phenotypic characteristics of the clinically encountered members of Scedosporium spp. and Lomentospora prolificans 241
Lomentospora prolificans (formerly Scedosporium prolificans) 242
Verruconis gallopava (formerly Ochroconis gallopava) 244
Table 2.16 Characteristics of some of the “black yeasts” 246
Exophiala jeanselmei species complex 247
Exophiala dermatitidis 249
Hortaea werneckii 251
Madurella mycetomatis 252
Trematosphaeria grisea (formerly Madurella grisea) 253
Piedraia hortae 254
Aureobasidium pullulans 255
Table 2.17 Differential characteristics of Aureobasidium pullulans versus Hormonema dematioides 257
Hormonema dematioides 258
Neoscytalidium dimidiatum 259
Botrytis cinerea 261
Stachybotrys chartarum 262
Thermothelomyces thermophilus (formerly Myceliophthora thermophila) 264
Curvularia spp. 265
Table 2.18 Characteristics of Curvularia spp. and Exserohilum rostratum 269
Exserohilum rostratum 270
Helminthosporium spp. 272
Alternaria spp. 273
Stemphylium spp. 275
Pseudopithomyces spp. (formerly Pithomyces spp.) 276
Epicoccum spp. 277
Nigrospora spp. 279
Chaetomium spp. 280
Phoma spp. 282
Dermatophytes 285
Introduction to Dermatophytes 287
Latin Terms for Dermatophyte Infections 288
Microsporum audouinii 289
Microsporum canis 290
Paraphyton cookei species complex (formerly Microsporum cookei species complex) 292
Nannizzia gypsea species complex (formerly Microsporum gypseum species complex) 293
Lophophyton gallinae (formerly Microsporum gallinae [zoophilic form] and Microsporum vanbreuseghemii [geophilic form]) 295
Nannizzia nana (formerly Microsporum nanum) 297
Microsporum ferrugineum 299
Trichophyton mentagrophytes species complex 300
Table 2.19 Differentiation of similar conidia-producing Trichophyton spp. and Arthroderma spp. 302
Trichophyton rubrum 303
Trichophyton tonsurans 305
Arthroderma terrestre species complex (formerly Trichophyton terrestre species complex) 307
Trichophyton megninii 308
Trichophyton soudanense 309
Table 2.20 Growth patterns of Trichophyton spp. and Arthroderma spp. on nutritional test media 310
Trichophyton schoenleinii 311
Trichophyton verrucosum 312
Trichophyton violaceum 313
Arthroderma uncinatum (formerly Trichophyton ajelloi) 314
Epidermophyton floccosum 315
Hyaline Hyphomycetes 317
Introduction to Hyaline Hyphomycetes 319
Fungi in Which Arthroconidia Predominate
Table 2.21 Differential characteristics of fungi in which arthroconidia predominate 320
Malbranchea spp. 321
Pseudogymnoascus pannorum (formerly Geomyces pannorum) 323
Arthrographis kalrae 324
Hormographiella aspergillata 326
Common Species of Aspergillus
The genus Aspergillus 327
Table 2.22 Differentiating characteristics of the most common Aspergillus spp. 329
Aspergillus fumigatus species complex 331
Aspergillus niger species complex 333
Aspergillus flavus species complex 334
Aspergillus versicolor species complex 336
Aspergillus ustus species complex 338
Aspergillus tanneri 340
Aspergillus nidulans species complex 342
Aspergillus glaucus 344
Aspergillus terreus species complex 345
Aspergillus clavatus 347
Other Common Hyaline Hyphomycetes
Penicillium spp. 348
Paecilomyces variotii 350
Rasamsonia argillacea species complex (formerly Geosmithia argillacea) 351
Purpureocillium lilacinum (formerly Paecilomyces lilacinus) 352
Table 2.23 Differential characteristics of Paecilomyces variotii, Rasamsonia argillacea, and Purpureocillium lilacinum 354
Scopulariopsis spp. 355
Table 2.24 Differential characteristics of Scopulariopsis brevicaulis versus Scopulariopsis brumptii 357
Gliocladium spp. 358
Trichoderma spp. 359
Metarhizium anisopliae species complex 361
Beauveria bassiana 363
Verticillium spp. 364
Acremonium and Sarocladium spp. 365
Fusarium spp. 367
Coniochaeta spp. (formerly Lecythophora spp.) 369
Trichothecium roseum 370
Chrysosporium spp. 371
Table 2.25 Differential characteristics of Chrysosporium versus Sporotrichum 373
Sporotrichum pruinosum 374
Sepedonium spp. 376
Chrysonilia sitophila 377
Schizophyllum commune 378
Part III Basics of Molecular Methods for Fungal Identification 379
Introduction 381
Fungal Targets 383
Table 3.1 Frequently used fungal molecular targets and primers for sequence-based species identification 385
Table 3.2 Examples of fungal molecular targets and primers for multilocus sequence-based species identification 386
Classic Molecular Identification Methods 387
Polymerase Chain Reaction 387
Non-Sequencing-Based Identification Methods 389
MALDI-TOF Mass Spectrometry 389
Signal Amplification Methods 390
PNA FISH 390
Nucleic Acid Amplification Methods 390
T2 Magnetic Resonance 390
Broad-Panel Molecular Testing and Other Emerging Sample-to-Answer Technologies 391
Sequencing-Based Identification Methods 393
Sanger Sequencing 393
Table 3.3 Lane construction for traditional bidirectional Sanger sequencing 394
Massive Parallel or Next-Generation Sequencing 394
Applications of DNA Sequencing 397
Accurate Molecular Identification 397
Table 3.4 Commonly used databases for identification of medically important fungi 398
Phylogenetic Analysis 399
Organism Typing 401
Detection of Genetic Determinants of Resistance 401
Part IV Laboratory Technique 403
Laboratory Procedures 405
Collection and Preparation of Specimens 406
Table 4.1 Common clinical sites for laboratory recovery of pathogenic fungi 409
Methods for Direct Microscopic Examination of Specimens 414
Primary Isolation 416
Table 4.2 Media for primary isolation of fungi 417
Macroscopic Examination of Cultures 419
Microscopic Examination of Growth 419
Procedure for Identification of Yeasts 421
Isolation of Yeast When Mixed with Bacteria 424
Germ Tube Test for the Presumptive Identification of Candida albicans 425
Rapid Enzyme Tests for the Presumptive Identification of Candida albicans 426
Caffeic Acid Disk Test 426
Olive Oil Disks for Culturing Malassezia spp. 426
Conversion of Thermally Dimorphic Fungi in Culture 427
Sporulation Inducement Method for Apophysomyces and Saksenaea 428
In vitro Hair Perforation Test (for Differentiation of Trichophyton mentagrophytes and Trichophyton rubrum) 428
Temperature Tolerance Testing 429
Maintenance of Stock Fungal Cultures 429
Controlling Mites 430
Staining Methods 431
Acid-Fast Modified Kinyoun Stain for Nocardia spp. 432
Acid-Fast Stain for Ascospores 433
Ascospore Stain 433
Calcofluor White Stain 434
Giemsa Stain 435
Gomori Methenamine Silver (GMS) Stain 435
Gram Stain (Hucker Modification) 438
Lactophenol Cotton Blue 439
Lactophenol Cotton Blue with Polyvinyl Alcohol (PVA) (Huber’s PVA Mounting
Medium, Modified) 439
Rehydration of Paraffin-Embedded Tissue (Deparaffination) 440
Media 441
Ascospore Media 443
Assimilation Media (for Yeasts) 444
Birdseed Agar (Niger Seed Agar; Staib Agar) 448
Brain Heart Infusion (BHI) Agar 449
Buffered Charcoal-Yeast Extract (BCYE) Agar 450
Canavanine Glycine Bromothymol Blue (CGB) Agar 450
Casein Agar 451
CHROMagar Candida Medium 452
CHROMagar Candida Plus Medium 453
CHROMID Candida Agar 453
Chromogenic Candida Agar (Brilliance Candida Agar) 454
Cornmeal Agar 454
Dermatophyte Test Medium (DTM) 455
Esculin Agar 456
Fermentation Broth for Yeasts 456
Inhibitory Mould Agar (IMA) 457
Leeming-Notman Agar (Modified) 458
Lysozyme Medium 458
Mycosel Agar 459
Potato Dextrose Agar and Potato Flake Agar 460
Rapid Assimilation of Trehalose (RAT) Broth 460
Sabouraud Brain Heart Infusion Agar (SABHI Agar) 462
Sabouraud Dextrose Agar (SDA) 463
Sabouraud Dextrose Agar with 15% Na Cl 464
Sabouraud Dextrose Broth 464
Starch Hydrolysis Agar 464
Trichophyton Agars 465
Tyrosine Agar 466
Urea Agar 467
Water Agar 467
Image Appendix 469
Glossary 477
References Cited 489
Index 507
O autorze
Lars F. Westblade, Ph D, D(ABMM) is the Director of the Clinical Microbiology Service at New York-Presbyterian/Weill Cornell Medical Center and Associate Professor at Weill Cornell Medicine with a primary appointment in the Department of Pathology and Laboratory Medicine and a secondary appointment in the Division of Infectious Diseases, Department of Medicine. He earned his doctoral degree from the University of Birmingham in the United Kingdom, and completed a fellowship in medical and public health laboratory microbiology at Washington University School of Medicine in St. Louis.
Eileen M. Burd, Ph D, D(ABMM) is the Director of the Clinical Microbiology Laboratory at Emory University Hospital and Professor at Emory University School of Medicine with a primary appointment in the Department of Pathology and Laboratory Medicine and a secondary appointment in the Department of Medicine, Division of Infectious Diseases. She earned her doctoral degree from the Medical College of Wisconsin in Milwaukee and was the Division Head of Microbiology at Henry Ford Hospital in Detroit, Michigan prior to joining the faculty at Emory University in 2007.
Shawn R. Lockhart, Ph D, D(ABBM) FAAM is the Senior Clinical Laboratory Advisor in the Mycotic Diseases Branch at the Centers for Disease Control and Prevention. He earned his doctoral degree from the University of Kentucky and completed his clinical microbiology fellowship at the University of Iowa Hospitals and Clinics. He directs the CDC training course in mold identification.
Gary W. Procop, MD, MS is the CEO of the American Board of Pathology and Professor of Pathology at the Cleveland Clinic Lerner School of Medicine. He remains a Consulting Staff for the Institute of Pathology and Laboratory Medicine, where he served as Medical Director for the Mycology Laboratory for more than two decades. He earned his doctoral degree from the Marshall University School of Medicine. His residency in anatomic and clinical pathology was completed at Duke University and his medical microbiology fellowship at the Mayo Clinic.