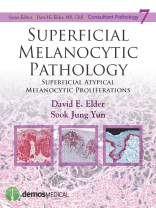
Add Expert Analysis of Difficult Cases to Your Practice With Consultant Pathology
Superficial Melanocytic Pathology provides expert guidance for resolving the real world problems pathologists face when diagnosing melanomas and other atypical pigmented lesions. It reviews each major category of atypical melanocytic lesions, including the pathology of the superficial categories of melanoma followed by a discussion of the major simulants of melanoma.
The book provides an overview of the morphologic description and diagnostic issues for each lesion, followed by 60 detailed, abundantly illustrated case presentations, offering an expert approach to diagnosis for a range of challenging cases. Five hundred high-quality color images support the case presentations. Of special interest is a chapter on ìambiguousî lesions of uncertain significance. The bookís thorough analysis of challenging lesions will aid pathologists in differentiating between benign superficial proliferations and malignant melanocytic tumors.
All Consultant Pathology Titles Provide:
- ACTUAL consultation cases and expert analysis
- EXPERT analysis provides a detailed discussion of the reasoning behind the diagnosis of each case
- COMPREHENSIVE coverage of challenging diagnoses
- CASES that are richly illustrated with high-quality photomicrographs
Mục lục
Series Foreword
Preface
Acknowledgments
Introduction
1.0 ‘Low CSD’ Superficial Atypical Melanocytic Proliferations (SAMP)
1.1 Superficial Spreading Melanoma
References
1.1.1 SSM Thin Mitogenic Versus Atypical Nevus With Mitoses
1.1.2 Thin Mitogenic Melanoma Versus Nevus With Mitoses
1.1.3 SSM With Extensive Regression Versus Regressing Nevus (Halo Nevus)
1.1.4 Thin SSM Versus Pagetoid Spitz Tumor in a Child
1.1.5 SSM Versus LMM Versus Atypical Nevus
1.1.6 Severely Dysplastic Nevus Versus Melanoma
1.1.7 SSM In Situ Versus SAMPUS—Severe Dysplasia
1.1.8 SSM Versus Pagetoid Spitz Tumor
1.2 Nevi Including Dysplastic Nevi
References
1.2.1 Epithelioid Cell Melanocytic Dysplasia Versus Superficial Spreading Melanoma
1.2.2 Moderate Versus Severe Dysplasia
1.2.3 Mild Dysplasia Versus Junctional Nevus
1.2.4 Severe Dysplasia Versus Nevoid Melanoma
1.2.5 Severe Dysplasia Versus Melanoma
1.2.6 Severe Dysplasia Versus Melanoma In Situ
1.2.7 Fibrosing Dysplastic Nevus Versus Melanoma With Regression
1.2.8 Dysplastic Nevus or Not?
1.2.9 Severe Dysplasia Versus Melanoma
1.2.10 Fibrosing Dysplastic Nevus Versus Regressing Melanoma
1.3 Recurrent and Traumatized Nevi
References
1.3.1 Recurrent Nevus Versus Melanoma
1.3.2 Recurrent and Traumatized Nevi
1.3.3 Recurrent Nevus Versus Melanoma
1.3.4 Recurrent Nevus Versus Melanoma
1.3.5 Recurrent and Traumatized Nevi
1.3.6 Nevus Versus Melanoma
2.0 High Chronic Solar Damage Superficial Atypical Melanocytic Proliferations
2.1 Lentigo Maligna Melanoma (High CSD Melanoma)
References
2.1.1 Lentigo Maligna Melanoma and Possible Precursor Lesions
2.1.2 Lentigo Maligna Melanoma With Desmoplastic Vertical Growth Phase Versus Atypical Neurotized Compound Nevus
2.1.3 Intraepidermal Atypical Melanocytic Proliferation of Uncertain Significance, Regressing Melanoma Versus Benign Lichenoid Keratosis With Junctional Melanocytic Hyperplasia Versus Atypical Nevus
2.1.4 Lentigo Maligna Melanoma, Invasive, Versus Incidental Dermal Nevus in Lentigo Maligna
2.1.5 Nevoid Lentigo Maligna Versus Severely Dysplastic Nevus
2.1.6 Nevoid Lentigo Maligna Versus Atypical Lentiginous Junctional Nevus
2.1.7 Melanoma In Situ Versus Lentiginous Nevus With Atypia or Severe Dysplasia
2.1.8 Melanoma In Situ Versus Severe Dysplasia
2.2 Actinic (Solar) Lentigo and Lentiginous Nevi in Sun-Damaged Skin
References
2.2.1 Actinic Lentigo Versus Lentigo Maligna
2.2.2 Actinic Lentigo Versus Lentigo Maligna
2.2.3 Actinic Lentigo With Spindle Cells
2.2.4 Atypical Lentigo Versus Regressing Melanoma
2.2.5 Lentiginous Nevus Versus Lentiginous Melanoma
3.0 Superficial Atypical Melanocytic Proliferations in Acral Skin
3.1 Acral Melanoma
References
3.1.1 Acral Melanoma Versus Acral Nevus
3.1.2 Acral Melanoma In Situ Versus Atypical Melanocytic Hyperplasia
3.1.3 Acral-Lentiginous Melanoma
3.1.4 Acral Melanoma Present at Specimen Margin
3.1.5 Acral Melanoma With Multiple Recurrences
3.1.6 Acral Junctional Nevus Versus Acral Melanoma
3.2 Special Site Nevi and Other Atypical Proliferations of Acral Skin
References
3.2.1 Acral-Lentiginous Nevus Versus Acral-Lentiginous Melanoma In Situ
3.2.2 Acral-Lentiginous Nevus Versus Acral-Lentiginous Melanoma
3.2.3 Acral Nevus Versus Dysplastic Nevus Versus Melanoma
3.2.4 Acral Versus Spitz Versus Dysplastic Nevus
3.2.5 Acral Nevus Versus Lentigo, Atypical
3.2.6 Acral Nevus Versus Lentigo
3.2.7 Atypical Nevus Versus Melanoma
4.0 Vulvar Melanomas, Nevi, and Lentigines
4.1 Vulvar Melanoma
References
4.1.1 Malignant Melanoma Versus Inflamed Atypical Nevus
4.1.2 Malignant Melanoma Versus Atypical Genital Nevus
4.1.3 Malignant Melanoma Versus Atypical Nevus
4.1.4 Vaginal Melanoma Versus Atypical Nevus
4.1.5 Vulvar Melanoma Versus Atypical Nevus
4.2 Special Site Nevi and Other Atypical Proliferations of Genital Skin
References
4.2.1 Compound Nevus Versus Dysplastic Nevus
4.2.2 Dysplastic Nevus Versus Special Site Nevus
4.2.3 Vulvar Nevi Versus Melanoma
4.2.4 Atypical Nevus Versus Melanoma
4.2.5 Spindle Cell Nevus Versus Melanoma
4.2.6 Vulvar Nevus Versus Dysplastic Nevus Versus Melanoma
5.0 Superficial Atypical Melanocytic Proliferations of Special Sites
References
5.0.1 Severe Melanocytic Dysplasia Versus Evolving Melanoma In Situ Versus Special Site Nevus of the Skin of the Breast
5.0.2 Special Site Nevus Versus Dysplastic Nevus
5.0.3 Special Site Nevus Versus Dysplastic Nevus Versus Melanoma
5.0.4 Special Site Nevus Versus Traumatized Nevus Versus Dysplastic Nevus Versus Melanoma
5.0.5 Special Site Nevus Versus Dysplastic Nevus Versus Melanoma
5.0.6 Special Site Nevus Versus Dysplastic Nevus
5.0.7 Special Site Nevus Versus Severely Dysplastic Nevus
5.0.8 Special Site Nevus Versus Dysplastic Nevus
5.0.9 Special Site Nevus Versus Severely Dysplastic Nevus or Melanoma of the Ear
6.0 Superficial Atypical Melanocytic Proliferations in Congenital Nevi
References
6.0.1 A Congenital Lesion on the Foot of a Two-Year-Old Child
6.0.2 Congenital Nevus Versus Congenital Pattern Nevus With Dysplasia
6.0.3 Congenital Pattern Nevus With Atypia-Reactive Versus Dysplastic
6.0.4 Dysplastic Nevus Versus Melanoma Arising in a Nevus
6.0.5 Atypical Congenital Nevus Versus Melanoma
7.0 Superficial Proliferations of Spindle and/or Epithelioid Melanocytes
7.1 Superficial Pagetoid and Atypical Spitzoid Proliferations
References
7.1.1 Atypical Pagetoid Spitz Tumor Versus Spitzoid Melanoma
7.1.2 Atypical Spitz Tumor Versus Pagetoid Melanoma
7.1.3 Atypical Spitz Tumor Versus Spitzoid Melanoma
7.1.4 Melanocytic Tumor of Uncertain Malignant Potential, Atypical Spitz Tumor Versus Spitzoid Melanoma
7.1.5 Melanocytic Tumor of Uncertain Malignant Potential, Favor Atypical Spitz Tumor Versus Favor Spitzoid Melanoma
7.1.6 Pagetoid Spitz Tumor Versus Superficial Spreading Melanoma
7.2 Pigmented Spindle Cell Nevi
References
7.2.1 Pigmented Spindle Cell Nevus Versus Pagetoid Spitz Versus Superficial Spreading Melanoma
7.2.2 Atypical Pigmented Spindle Cell Nevus Versus Superficial Spreading Melanoma Versus Severely Dysplastic Nevus
7.2.3 Pigmented Spindle Cell Nevus Versus Severe Dysplasia or Evolving Melanoma In Situ
7.2.4 Pigmented Spindle Cell Nevus Versus Pigmented Spitz Nevus Versus Severely Dysplastic Nevus
7.2.5 Superficial Atypical Melanocytic Proliferation of Uncertain Significance, Pigmented Spindle Cell Nevus Versus Spindle Cell Melanoma
Index
Giới thiệu về tác giả
David E. Elder, MB, Ch B, is Professor of Pathology and Laboratory Medicine and Vice Chair for Anatomic Pathology at the Hospital of the University of Pennsylvania.